| << Chapter < Page | Chapter >> Page > |
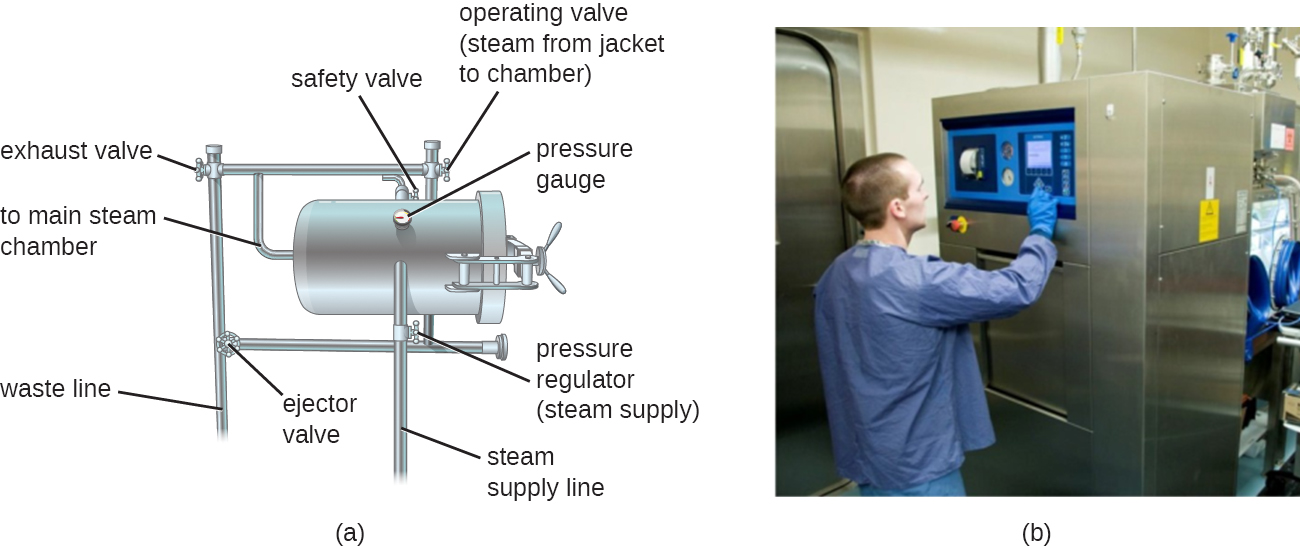
Autoclaves rely on moist-heat sterilization. They are used to raise temperatures above the boiling point of water to sterilize items such as surgical equipment from vegetative cells, viruses, and especially endospores, which are known to survive boiling temperatures, without damaging the items. Charles Chamberland (1851–1908) designed the modern autoclave in 1879 while working in the laboratory of Louis Pasteur . The autoclave is still considered the most effective method of sterilization ( [link] ). Outside laboratory and clinical settings, large industrial autoclaves called retort s allow for moist-heat sterilization on a large scale.
In general, the air in the chamber of an autoclave is removed and replaced with increasing amounts of steam trapped within the enclosed chamber, resulting in increased interior pressure and temperatures above the boiling point of water. The two main types of autoclaves differ in the way that air is removed from the chamber. In gravity displacement autoclave s, steam is introduced into the chamber from the top or sides. Air, which is heavier than steam, sinks to the bottom of the chamber, where it is forced out through a vent. Complete displacement of air is difficult, especially in larger loads, so longer cycles may be required for such loads. In prevacuum sterilizer s, air is removed completely using a high-speed vacuum before introducing steam into the chamber. Because air is more completely eliminated, the steam can more easily penetrate wrapped items. Many autoclaves are capable of both gravity and prevacuum cycles, using the former for the decontamination of waste and sterilization of media and unwrapped glassware, and the latter for sterilization of packaged instruments.
Standard operating temperatures for autoclaves are 121 °C or, in some cases, 132 °C, typically at a pressure of 15 to 20 pounds per square inch (psi). The length of exposure depends on the volume and nature of material being sterilized, but it is typically 20 minutes or more, with larger volumes requiring longer exposure times to ensure sufficient heat transfer to the materials being sterilized. The steam must directly contact the liquids or dry materials being sterilized, so containers are left loosely closed and instruments are loosely wrapped in paper or foil. The key to autoclaving is that the temperature must be high enough to kill endospores to achieve complete sterilization.
Because sterilization is so important to safe medical and laboratory protocols, quality control is essential. Autoclaves may be equipped with recorders to document the pressures and temperatures achieved during each run. Additionally, internal indicators of various types should be autoclaved along with the materials to be sterilized to ensure that the proper sterilization temperature has been reached ( [link] ). One common type of indicator is the use of heat-sensitive autoclave tape , which has white stripes that turn black when the appropriate temperature is achieved during a successful autoclave run. This type of indicator is relatively inexpensive and can be used during every run. However, autoclave tape provides no indication of length of exposure, so it cannot be used as an indicator of sterility. Another type of indicator, a biological indicator spore test, uses either a strip of paper or a liquid suspension of the endospores of Geobacillus stearothermophilus to determine whether the endospores are killed by the process. The endospores of the obligate thermophilic bacterium G. stearothermophilus are the gold standard used for this purpose because of their extreme heat resistance. Biological spore indicators can also be used to test the effectiveness of other sterilization protocols, including ethylene oxide, dry heat, formaldehyde, gamma radiation, and hydrogen peroxide plasma sterilization using either G . stearothermophilus , Bacillus atrophaeus, B. subtilis, or B. pumilus spores. In the case of validating autoclave function, the endospores are incubated after autoclaving to ensure no viable endospores remain. Bacterial growth subsequent to endospore germination can be monitored by biological indicator spore tests that detect acid metabolites or fluorescence produced by enzymes derived from viable G. stearothermophilus . A third type of autoclave indicator is the Diack tube , a glass ampule containing a temperature-sensitive pellet that melts at the proper sterilization temperature. Spore strips or Diack tubes are used periodically to ensure the autoclave is functioning properly.

Notification Switch
Would you like to follow the 'Microbiology' conversation and receive update notifications?