| << Chapter < Page | Chapter >> Page > |
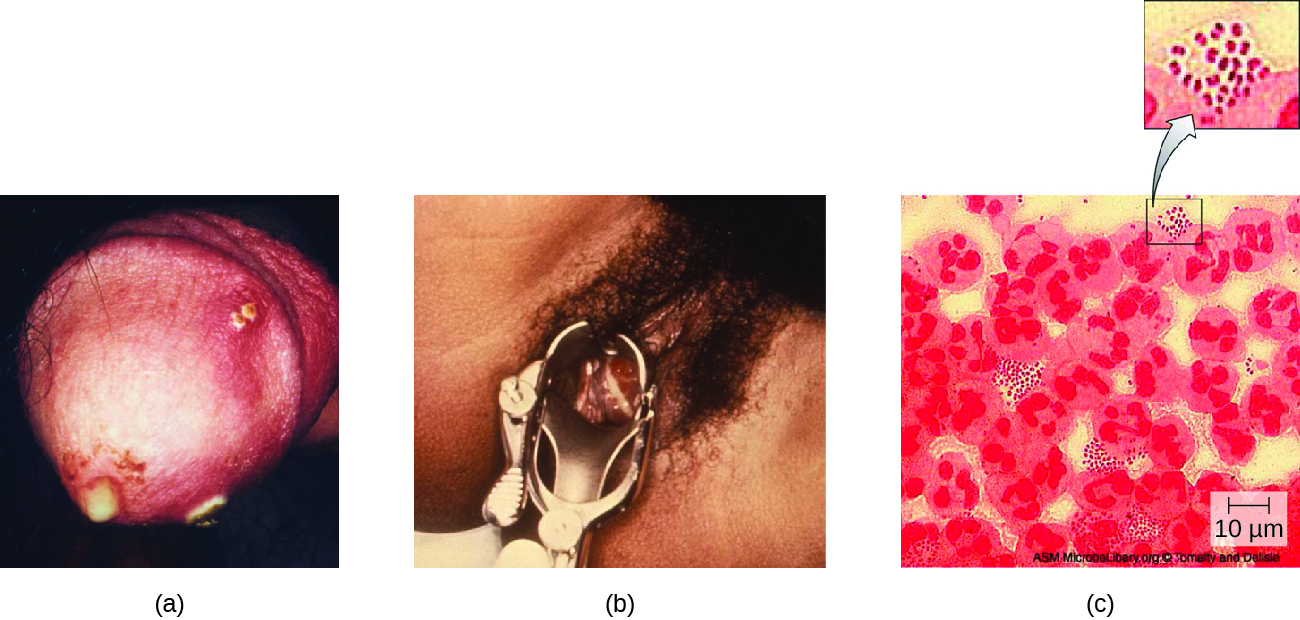
Women may develop pelvic pain, discharge from the vagina, intermenstrual bleeding (i.e., bleeding not associated with normal menstruation), and pain or irritation associated with urination. As with men, the infection can become chronic. In women, however, chronic infection can cause increases in menstrual flow. Rectal infection can also occur, with the symptoms previously described for men. Infections that spread to the endometrium and fallopian tubes can cause pelvic inflammatory disease (PID) , characterized by pain in the lower abdominal region, dysuria , vaginal discharge, and fever. PID can also lead to infertility through scarring and blockage of the fallopian tubes ( salpingitis ); it may also increase the risk of a life-threatening ectopic pregnancy , which occurs when a fertilized egg begins developing somewhere other than the uterus (e.g., in the fallopian tube or ovary).
When a gonorrhea infection disseminates throughout the body, serious complications can develop. The infection may spread through the blood ( bacteremia ) and affect organs throughout the body, including the heart ( gonorrheal endocarditis ), joints ( gonorrheal arthritis ), and meninges encasing the brain ( meningitis ).
Urethritis caused by N. gonorrhoeae can be difficult to treat due to antibiotic resistance (see Micro Connections ). Some strains have developed resistance to the fluoroquinolones , so cephalosporins are often a first choice for treatment. Because co-infection with C. trachomatis is common, the CDC recommends treating with a combination regimen of ceftriaxone and azithromycin . Treatment of sexual partners is also recommended to avoid reinfection and spread of infection to others. Centers for Disease Control and Prevention. “2015 Sexually Transmitted Diseases Treatment Guidelines: Gonococcal Infections,” 2015. http://www.cdc.gov/std/tg2015/gonorrhea.htm.
Antibiotic resistance in many pathogens is steadily increasing, causing serious concern throughout the public health community. Increased resistance has been especially notable in some species, such as Neisseria gonorrhoeae . The CDC monitors the spread of antibiotic resistance in N. gonorrhoeae , which it classifies as an urgent threat, and makes recommendations for treatment. So far, N. gonorrhoeae has shown resistance to cefixime (a cephalosporin), ceftriaxone (another cephalosporin), azithromycin, and tetracycline. Resistance to tetracycline is the most common, and was seen in 188,600 cases of gonorrhea in 2011 (out of a total 820,000 cases). In 2011, some 246,000 cases of gonorrhea involved strains of N. gonorrhoeae that were resistant to at least one antibiotic. Centers for Disease Control and Prevention. “Antibiotic Resistance Threats in the United States, 2013,” 2013. http://www.cdc.gov/drugresistance/pdf/ar-threats-2013-508.pdf. These resistance genes are spread by plasmids, and a single bacterium may be resistant to multiple antibiotics. The CDC currently recommends treatment with two medications, ceftriaxone and azithromycin, to attempt to slow the spread of resistance. If resistance to cephalosporins increases, it will be extremely difficult to control the spread of N. gonorrhoeae .

Notification Switch
Would you like to follow the 'Microbiology' conversation and receive update notifications?