| << Chapter < Page | Chapter >> Page > |
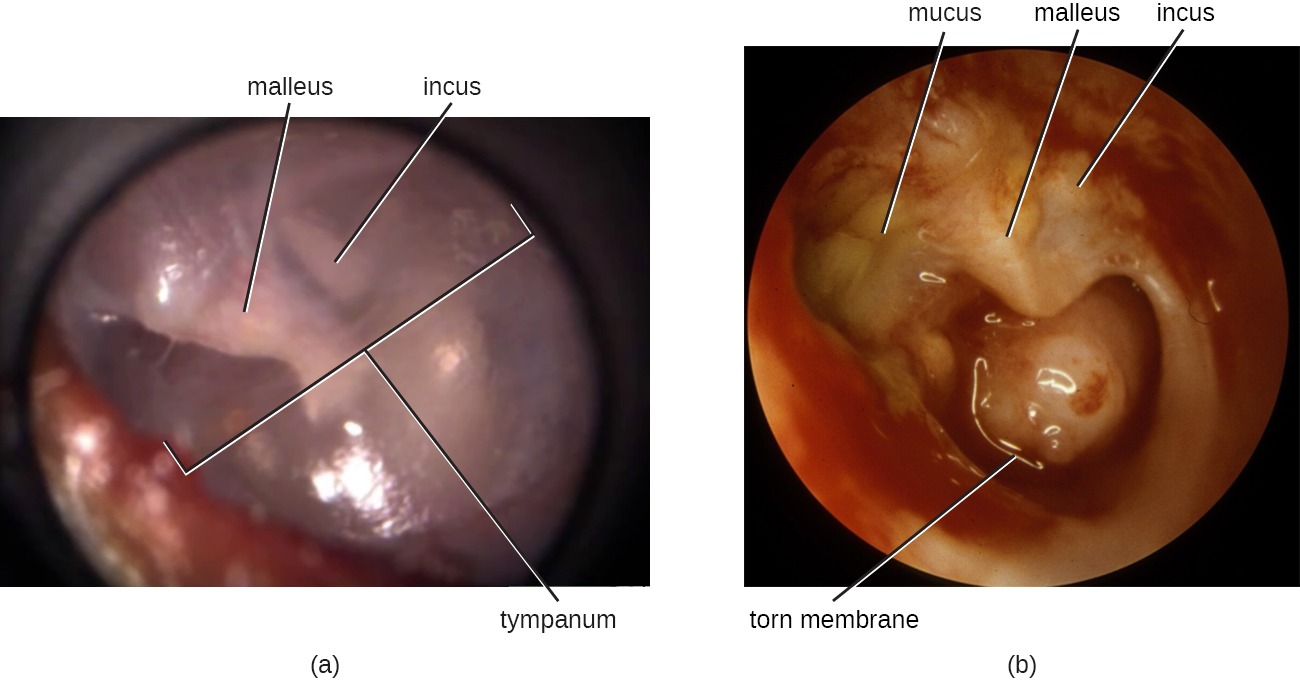
AOM can be caused by a variety of bacteria. Among neonates, S. pneumoniae is the most common cause of AOM, but Escherichia coli , Enterococcus spp., and group B Streptococcus species can also be involved. In older infants and children younger than 14 years old, the most common bacterial causes are S. pneumoniae , Haemophilus influenzae , or Moraxella catarrhalis . Among S. pneumoniae infections , encapsulated strains are frequent causes of AOM. By contrast, the strains of H. influenzae and M. cattarhalis that are responsible for AOM do not possess a capsule. Rather than direct tissue damage by these pathogens, bacterial components such as lipopolysaccharide (LPS) in gram-negative pathogens induce an inflammatory response that causes swelling, pus, and tissue damage within the middle ear ( [link] ).
Any blockage of the eustachian tubes, with or without infection, can cause fluid to become trapped and accumulate in the middle ear. This is referred to as otitis media with effusion (OME) . The accumulated fluid offers an excellent reservoir for microbial growth and, consequently, secondary bacterial infections often ensue. This can lead to recurring and chronic earaches, which are especially common in young children. The higher incidence in children can be attributed to many factors. Children have more upper respiratory infections, in general, and their eustachian tubes are also shorter and drain at a shallower angle. Young children also tend to spend more time lying down than adults, which facilitates drainage from the nasopharynx through the eustachian tube and into the middle ear. Bottle feeding while lying down enhances this risk because the sucking action on the bottle causes negative pressure to build up within the eustachian tube, promoting the movement of fluid and bacteria from the nasopharynx.
Diagnosis is typically made based on clinical signs and symptoms, without laboratory testing to determine the specific causative agent. Antibiotics are frequently prescribed for the treatment of AOM. High-dose amoxicillin is the first-line drug, but with increasing resistance concerns, macrolides and cephalosporin s may also be used. The pneumococcal conjugate vaccine (PCV13) contains serotypes that are important causes of AOM, and vaccination has been shown to decrease the incidence of AOM. Vaccination against influenza has also been shown to decrease the risk for AOM, likely because viral infections like influenza predispose patients to secondary infections with S. pneumoniae . Although there is a conjugate vaccine available for the invasive serotype B of H. influenzae , this vaccine does not impact the incidence of H. influenzae AOM. Because unencapsulated strains of H. influenzae and M. catarrhalis are involved in AOM, vaccines against bacterial cellular factors other than capsules will need to be developed.

Notification Switch
Would you like to follow the 'Microbiology' conversation and receive update notifications?