| << Chapter < Page | Chapter >> Page > |
While people are often unaware of their sleep apnea, they are keenly aware of some of the adverse consequences of insufficient sleep. Consider a patient who believed that as a result of his sleep apnea he “had three car accidents in six weeks. They were ALL my fault. Two of them I didn’t even know I was involved in until afterwards” (Henry&Rosenthal, 2013, p. 52). It is not uncommon for people suffering from undiagnosed or untreated sleep apnea to fear that their careers will be affected by the lack of sleep, illustrated by this statement from another patient, “I’m in a job where there’s a premium on being mentally alert. I was really sleepy… and having trouble concentrating…. It was getting to the point where it was kind of scary” (Henry&Rosenthal, 2013, p. 52).
There are two types of sleep apnea: obstructive sleep apnea and central sleep apnea. Obstructive sleep apnea occurs when an individual’s airway becomes blocked during sleep, and air is prevented from entering the lungs. In central sleep apnea , disruption in signals sent from the brain that regulate breathing cause periods of interrupted breathing (White, 2005).
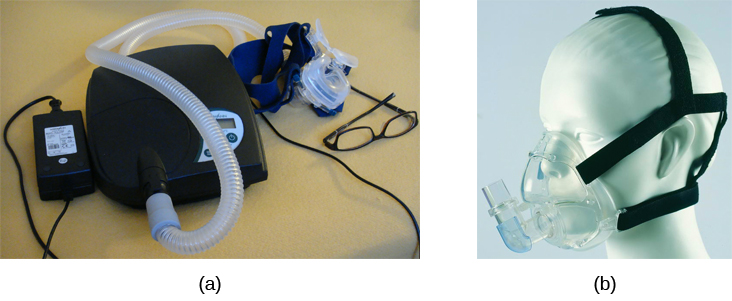
One of the most common treatments for sleep apnea involves the use of a special device during sleep. A continuous positive airway pressure (CPAP) device includes a mask that fits over the sleeper’s nose and mouth, which is connected to a pump that pumps air into the person’s airways, forcing them to remain open, as shown in [link] . Some newer CPAP masks are smaller and cover only the nose. This treatment option has proven to be effective for people suffering from mild to severe cases of sleep apnea (McDaid et al., 2009). However, alternative treatment options are being explored because consistent compliance by users of CPAP devices is a problem. Recently, a new EPAP (expiratory positive air pressure) device has shown promise in double-blind trials as one such alternative (Berry, Kryger,&Massie, 2011).
In sudden infant death syndrome (SIDS) an infant stops breathing during sleep and dies. Infants younger than 12 months appear to be at the highest risk for SIDS, and boys have a greater risk than girls. A number of risk factors have been associated with SIDS including premature birth, smoking within the home, and hyperthermia. There may also be differences in both brain structure and function in infants that die from SIDS (Berkowitz, 2012; Mage&Donner, 2006; Thach, 2005).
The substantial amount of research on SIDS has led to a number of recommendations to parents to protect their children ( [link] ). For one, research suggests that infants should be placed on their backs when put down to sleep, and their cribs should not contain any items which pose suffocation threats, such as blankets, pillows or padded crib bumpers (cushions that cover the bars of a crib). Infants should not have caps placed on their heads when put down to sleep in order to prevent overheating, and people in the child’s household should abstain from smoking in the home. Recommendations like these have helped to decrease the number of infant deaths from SIDS in recent years (Mitchell, 2009; Task Force on Sudden Infant Death Syndrome, 2011).

Notification Switch
Would you like to follow the 'Psychology' conversation and receive update notifications?