| << Chapter < Page | Chapter >> Page > |
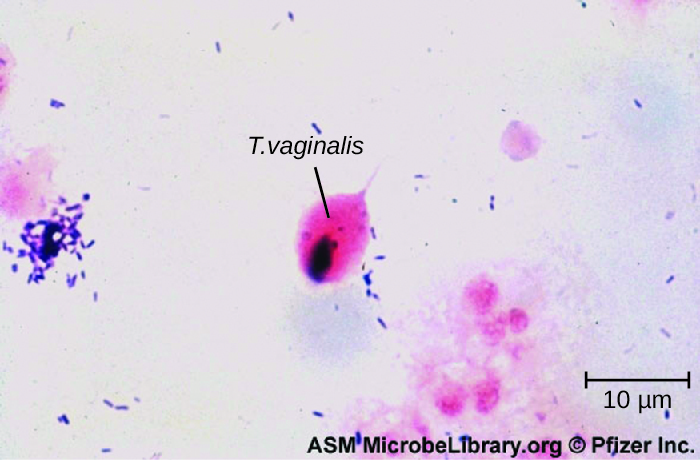
Only one major protozoan species causes infections in the urogenital system. Trichomoniasis , or “trich,” is the most common nonviral STI and is caused by a flagellated protozoan Trichomonas vaginalis . T. vaginalis has an undulating membrane and, generally, an amoeboid shape when attached to cells in the vagina. In culture, it has an oval shape.
T. vaginalis is commonly found in the normal microbiota of the vagina. As with other vaginal pathogens, it can cause vaginitis when there is disruption to the normal microbiota. It is found only as a trophozoite and does not form cysts. T. vaginalis can adhere to cells using adhesins such as lipoglycans ; it also has other cell-surface virulence factors, including tetraspanins that are involved in cell adhesion, motility, and tissue invasion. In addition, T. vaginalis is capable of phagocytosing other microbes of the normal microbiota, contributing to the development of an imbalance that is favorable to infection.
Both men and women can develop trichomoniasis. Men are generally asymptomatic, and although women are more likely to develop symptoms, they are often asymptomatic as well. When symptoms do occur, they are characteristic of urethritis. Men experience itching, irritation, discharge from the penis, and burning after urination or ejaculation. Women experience dysuria; itching, burning, redness, and soreness of the genitalia; and vaginal discharge. The infection may also spread to the cervix. Infection increases the risk of transmitting or acquiring HIV and is associated with pregnancy complications such as preterm birth.
Microscopic evaluation of wet mounts is an inexpensive and convenient method of diagnosis, but the sensitivity of this method is low ( [link] ). Nucleic acid amplification testing (NAAT) is preferred due to its high sensitivity. Using wet mounts and then NAAT for those who initially test negative is one option to improve sensitivity. Samples may be obtained for NAAT using urine, vaginal, or endocervical specimens for women and with urine and urethral swabs for men. It is also possible to use other methods such as the OSOM Trichomonas Rapid Test (an immunochromatographic test that detects antigen) and a DNA probe test for multiple species associated with vaginitis (the Affirm VPII Microbial Identification Test discussed in section 23.5). Association of Public Health Laboratories. “Advances in Laboratory Detection of Trichomonas vaginalis,” 2013. http://www.aphl.org/AboutAPHL/publications/Documents/ID_2013August_Advances-in-Laboratory-Detection-of-Trichomonas-vaginalis.pdf. T. vaginalis is sometimes detected on a Pap test , but this is not considered diagnostic due to high rates of false positives and negatives. The recommended treatment for trichomoniasis is oral metronidazole or tinidazole . Sexual partners should be treated as well.

Notification Switch
Would you like to follow the 'Microbiology' conversation and receive update notifications?