| << Chapter < Page | Chapter >> Page > |
A vaccine is available to protect individuals from anthrax. However, unlike most routine vaccines, the current anthrax vaccine is unique in both its formulation and the protocols dictating who receives it. Centers for Disease Control and Prevention . “Anthrax: Medical Care: Prevention: Antibiotics.” http://www.cdc.gov/anthrax/medical-care/prevention.html. Accessed Sept 14, 2016. The vaccine is administered through five intramuscular injections over a period of 18 months, followed by annual boosters. The US Food and Drug Administration (FDA) has only approved administration of the vaccine prior to exposure for at-risk adults, such as individuals who work with anthrax in a laboratory, some individuals who handle animals or animal products (e.g., some veterinarians), and some members of the United States military. The vaccine protects against cutaneous and inhalation anthrax using cell-free filtrates of microaerophilic cultures of an avirulent, nonencapsulated strain of B. anthracis . Emergent Biosolutions. AVA (BioThrax) vaccine package insert (Draft). Nov 2015. http://www.fda.gov/downloads/biologicsbloodvaccines/bloodbloodproducts/approvedproducts/licensedproductsblas/ucm074923.pdf. The FDA has not approved the vaccine for routine use after exposure to anthrax, but if there were ever an anthrax emergency in the United States, patients could be given anthrax vaccine after exposure to help prevent disease.
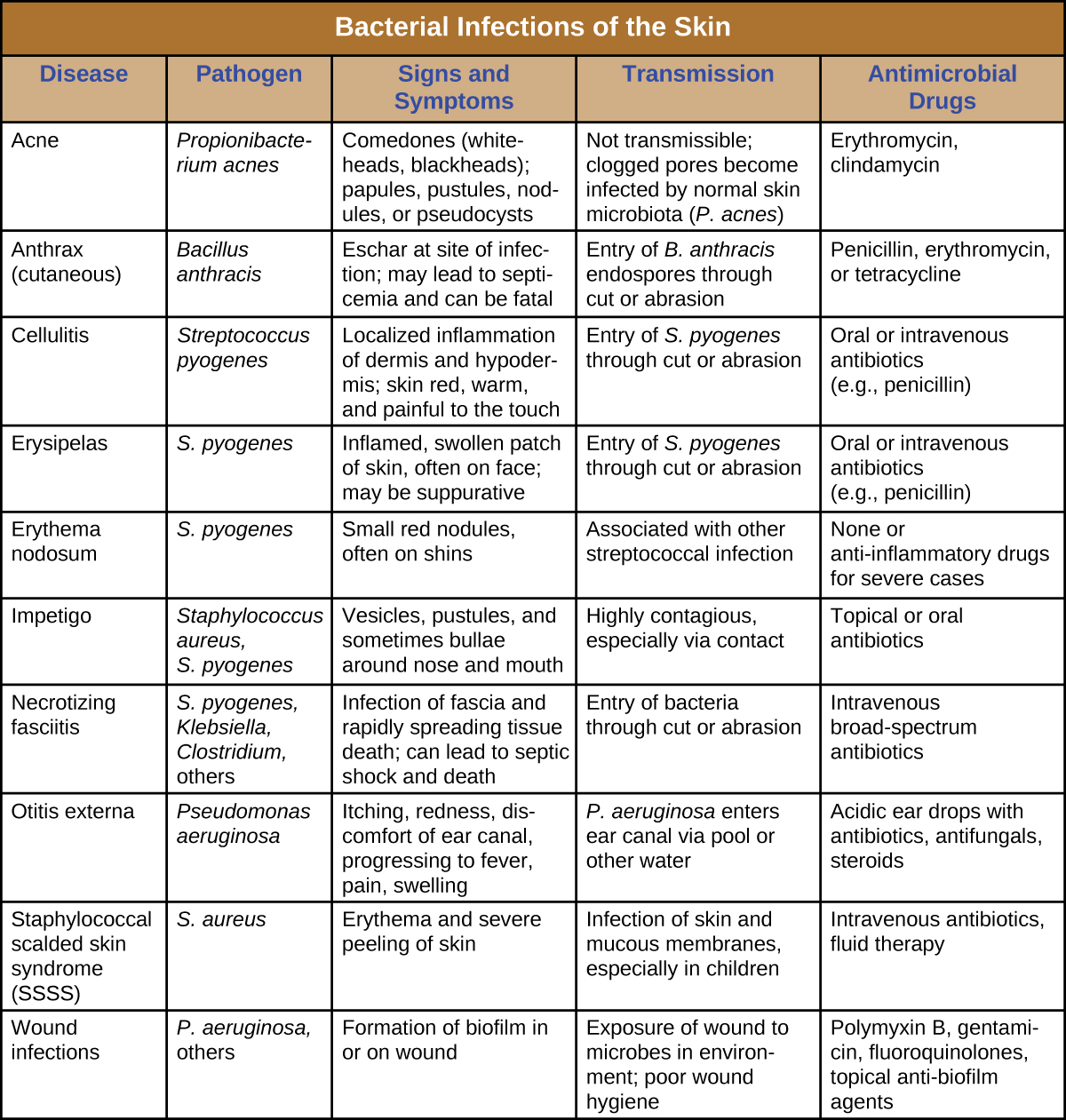
Bacterial infections of the skin can cause a wide range of symptoms and syndromes, ranging from the superficial and relatively harmless to the severe and even fatal. Most bacterial skin infections can be diagnosed by culturing the bacteria and treated with antibiotics. Antimicrobial susceptibility testing is also often necessary because many strains of bacteria have developed antibiotic resistance. [link] summarizes the characteristics of some common bacterial skin infections.
Like the skin, the surface of the eye comes in contact with the outside world and is somewhat prone to infection by bacteria in the environment. Bacterial conjunctivitis ( pinkeye ) is a condition characterized by inflammation of the conjunctiva, often accompanied by a discharge of sticky fluid (described as acute purulent conjunctivitis) ( [link] ). Conjunctivitis can affect one eye or both, and it usually does not affect vision permanently. Bacterial conjunctivitis is most commonly caused by Haemophilus influenzae , but can also be caused by other species such as Moraxella catarrhalis , S. pneumoniae, and S. aureus . The causative agent may be identified using bacterial cultures, Gram stain, and diagnostic biochemical, antigenic, or nucleic acid profile tests of the isolated pathogen. Bacterial conjunctivitis is very contagious, being transmitted via secretions from infected individuals, but it is also self-limiting. Bacterial conjunctivitis usually resolves in a few days, but topical antibiotics are sometimes prescribed. Because this condition is so contagious, medical attention is recommended whenever it is suspected. Individuals who use contact lenses should discontinue their use when conjunctivitis is suspected. Certain symptoms, such as blurred vision, eye pain, and light sensitivity, can be associated with serious conditions and require medical attention.

Notification Switch
Would you like to follow the 'Microbiology' conversation and receive update notifications?