| << Chapter < Page | Chapter >> Page > |
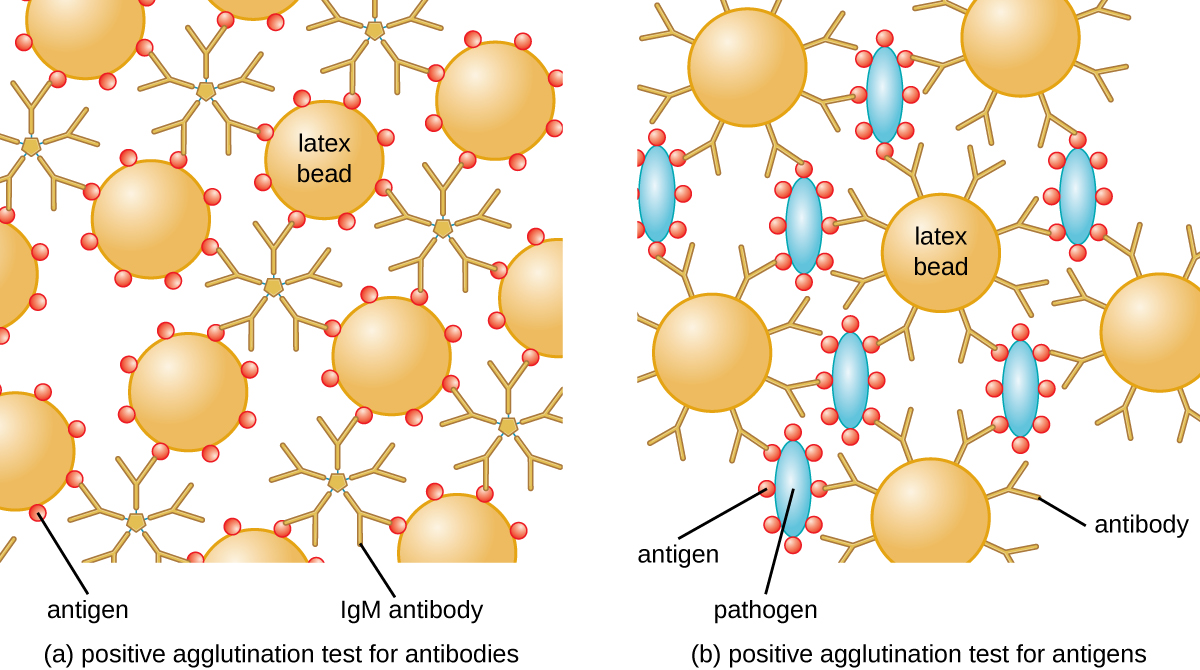
To identify antibodies in a patient’s serum, the antigen of interest is attached to latex beads. When mixed with patient serum, the antibodies will bind the antigen, cross-linking the latex beads and causing the beads to agglutinate indirectly; this indicates the presence of the antibody ( [link] ). This technique is most often used when looking for IgM antibodies, because their structure provides maximum cross-linking. One widely used example of this assay is a test for rheumatoid factor (RF) to confirm a diagnosis of rheumatoid arthritis. RF is, in fact, the presence of IgM antibodies that bind to the patient’s own IgG . RF will agglutinate IgG-coated latex beads.
In the reverse test, soluble antigens can be detected in a patient’s serum by attaching specific antibodies (commonly mAbs) to the latex beads and mixing this complex with the serum ( [link] ).
Agglutination tests are widely used in underdeveloped countries that may lack appropriate facilities for culturing bacteria. For example, the Widal test , used for the diagnosis of typhoid fever , looks for agglutination of Salmonella enterica subspecies typhi in patient sera. The Widal test is rapid, inexpensive, and useful for monitoring the extent of an outbreak; however, it is not as accurate as tests that involve culturing of the bacteria. The Widal test frequently produces false positives in patients with previous infections with other subspecies of Salmonella , as well as false negatives in patients with hyperproteinemia or immune deficiencies.
In addition, agglutination tests are limited by the fact that patients generally do not produce detectable levels of antibody during the first week (or longer) of an infection. A patient is said to have undergone seroconversion when antibody levels reach the threshold for detection. Typically, seroconversion coincides with the onset of signs and symptoms of disease. However, in an HIV infection, for example, it generally takes 3 weeks for seroconversion to take place, and in some instances, it may take much longer.
Similar to techniques for the precipitin ring test and plaque assays, it is routine to prepare serial two-fold dilutions of the patient’s serum and determine the titer of agglutinating antibody present. Since antibody levels change over time in both primary and secondary immune responses, by checking samples over time, changes in antibody titer can be detected. For example, a comparison of the titer during the acute phase of an infection versus the titer from the convalescent phase will distinguish whether an infection is current or has occurred in the past. It is also possible to monitor how well the patient’s immune system is responding to the pathogen.

Notification Switch
Would you like to follow the 'Microbiology' conversation and receive update notifications?