| << Chapter < Page | Chapter >> Page > |
The splitting of the C3 protein is the common step to both pathways. In the alternate pathway, C3 is activated spontaneously and, after reacting with the molecules factor P, factor B, and factor D, splits apart. The larger fragment, C3b, binds to the surface of the pathogen and C3a, the smaller fragment, diffuses outward from the site of activation and attracts phagocytes to the site of infection. Surface-bound C3b then activates the rest of the cascade, with the last five proteins, C5–C9, forming the membrane-attack complex (MAC). The MAC can kill certain pathogens by disrupting their osmotic balance. The MAC is especially effective against a broad range of bacteria. The classical pathway is similar, except the early stages of activation require the presence of antibody bound to antigen, and thus is dependent on the adaptive immune response. The earlier fragments of the cascade also have important functions. Phagocytic cells such as macrophages and neutrophils are attracted to an infection site by chemotactic attraction to smaller complement fragments. Additionally, once they arrive, their receptors for surface-bound C3b opsonize the pathogen for phagocytosis and destruction.
The hallmark of the innate immune response is inflammation . Inflammation is something everyone has experienced. Stub a toe, cut a finger, or do any activity that causes tissue damage and inflammation will result, with its four characteristics: heat, redness, pain, and swelling (“loss of function” is sometimes mentioned as a fifth characteristic). It is important to note that inflammation does not have to be initiated by an infection, but can also be caused by tissue injuries. The release of damaged cellular contents into the site of injury is enough to stimulate the response, even in the absence of breaks in physical barriers that would allow pathogens to enter (by hitting your thumb with a hammer, for example). The inflammatory reaction brings in phagocytic cells to the damaged area to clear cellular debris and to set the stage for wound repair ( [link] ).
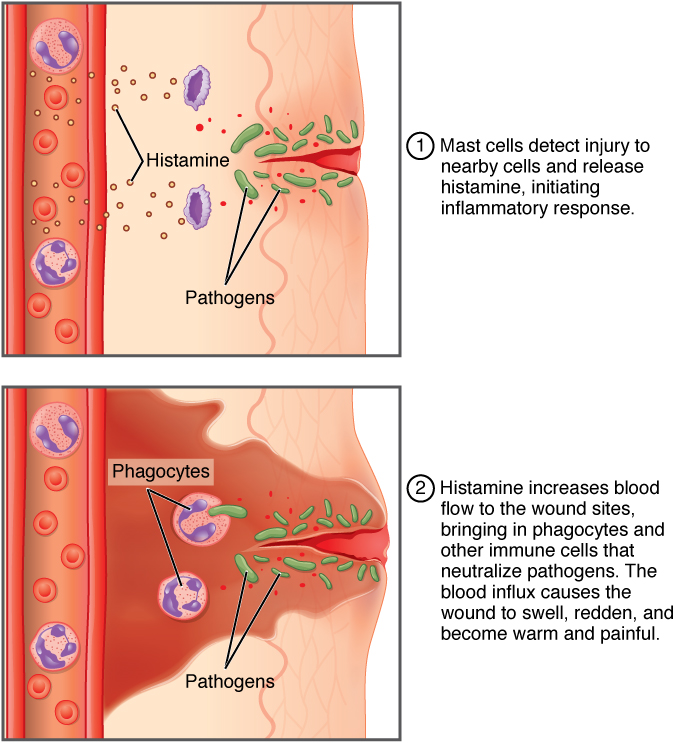
This reaction also brings in the cells of the innate immune system, allowing them to get rid of the sources of a possible infection. Inflammation is part of a very basic form of immune response. The process not only brings fluid and cells into the site to destroy the pathogen and remove it and debris from the site, but also helps to isolate the site, limiting the spread of the pathogen. Acute inflammation is a short-term inflammatory response to an insult to the body. If the cause of the inflammation is not resolved, however, it can lead to chronic inflammation, which is associated with major tissue destruction and fibrosis. Chronic inflammation is ongoing inflammation. It can be caused by foreign bodies, persistent pathogens, and autoimmune diseases such as rheumatoid arthritis.
There are four important parts to the inflammatory response:
Overall, inflammation is valuable for many reasons. Not only are the pathogens killed and debris removed, but the increase in vascular permeability encourages the entry of clotting factors, the first step towards wound repair. Inflammation also facilitates the transport of antigen to lymph nodes by dendritic cells for the development of the adaptive immune response.
Innate immune responses are critical to the early control of infections. Whereas barrier defenses are the body’s first line of physical defense against pathogens, innate immune responses are the first line of physiological defense. Innate responses occur rapidly, but with less specificity and effectiveness than the adaptive immune response. Innate responses can be caused by a variety of cells, mediators, and antibacterial proteins such as complement. Within the first few days of an infection, another series of antibacterial proteins are induced, each with activities against certain bacteria, including opsonization of certain species. Additionally, interferons are induced that protect cells from viruses in their vicinity. Finally, the innate immune response does not stop when the adaptive immune response is developed. In fact, both can cooperate and one can influence the other in their responses against pathogens.
Visit this website to learn about phagocyte chemotaxis. Phagocyte chemotaxis is the movement of phagocytes according to the secretion of chemical messengers in the form of interleukins and other chemokines. By what means does a phagocyte destroy a bacterium that it has ingested?
The bacterium is digested by the phagocyte’s digestive enzymes (contained in its lysosomes).

Notification Switch
Would you like to follow the 'Anatomy & Physiology' conversation and receive update notifications?